Pelvic Organ Prolapse Surgery
Helping You Feel Strong, Supported, and Comfortable Again
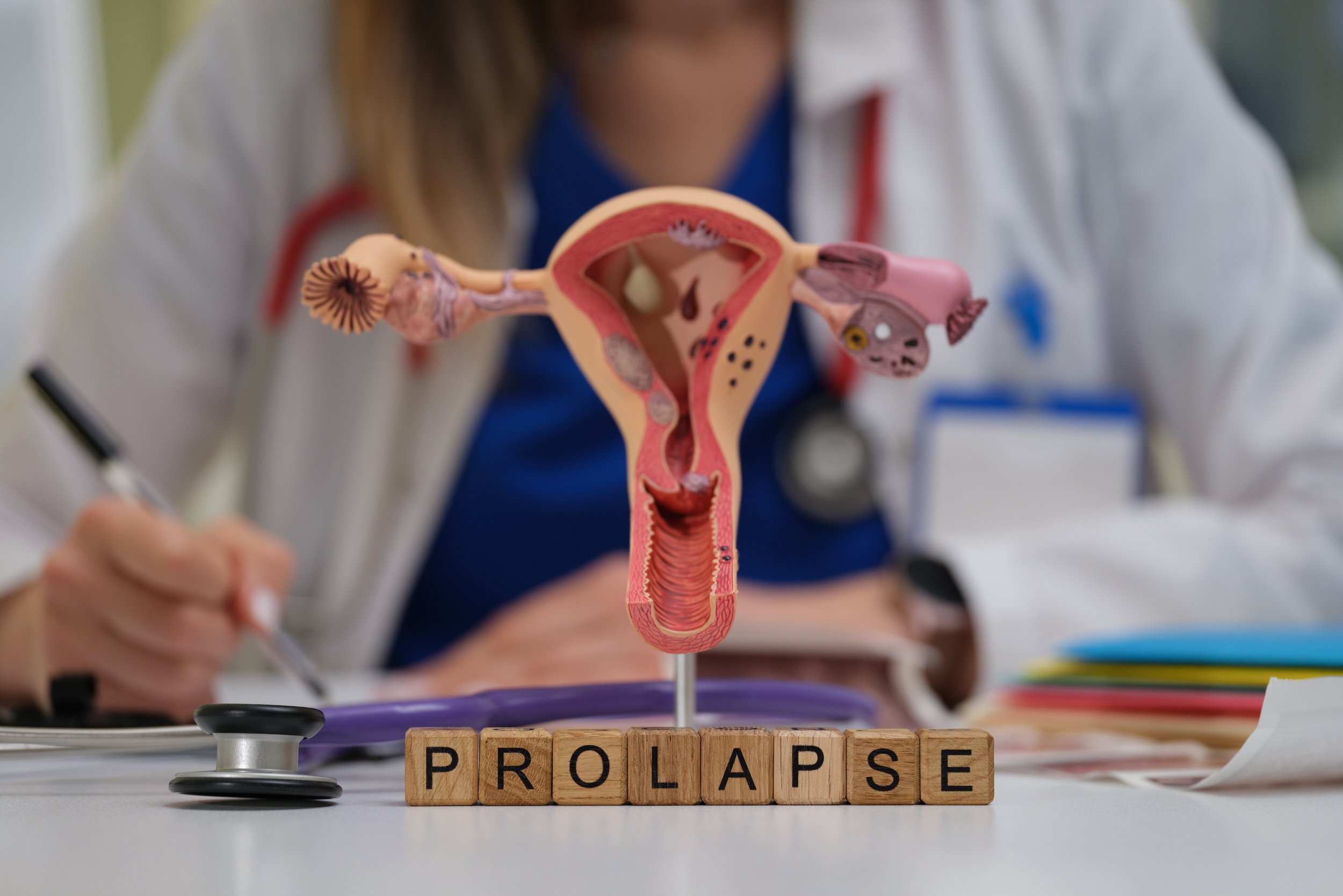
Pelvic organ prolapse is a common condition where the bladder, uterus, or rectum pushes into or out of the vaginal canal due to weakened pelvic floor muscles. It often occurs after childbirth, menopause, or pelvic surgery — and while it’s not dangerous, it can significantly affect comfort, physical activity, and quality of life. Dr. Affie Tourani offers compassionate, evidence-based care for prolapse, including non-surgical support and advanced surgical repair options that respect your lifestyle and future goals.
What Is Pelvic Organ Prolapse?
Prolapse occurs when the structures that hold the pelvic organs in place (muscles, ligaments, and fascia) become weakened or stretched. Depending on the organ affected, prolapse can be classified as:
Cystocele (bladder bulging into the front vaginal wall)
Rectocele (rectum bulging into the back vaginal wall)
Uterine prolapse (uterus descending into the vaginal canal)
Enterocele (small bowel pushing into the vaginal wall)
Vaginal vault prolapse (after hysterectomy)
Symptoms of Prolapse
Vaginal pressure or heaviness
A visible or palpable bulge at the vaginal opening
Discomfort when standing, walking, or lifting
Difficulty with bowel emptying
Sensation of looseness or “dragging” in the pelvis
Pain or discomfort during intimacy
Treatment Options
Non-Surgical Management
For mild to moderate prolapse, Dr. Tourani may recommend:
Pelvic floor physiotherapy to strengthen support muscles
Vaginal pessaries – small silicone devices inserted to support the organs
Lifestyle advice (weight management, avoiding straining, bowel care)
Surgical Options
When symptoms are bothersome and conservative measures are not enough, surgery can offer excellent symptom relief and long-term results. The types of surgeries offered include:
Anterior repair – strengthens the front vaginal wall to support the bladder
Posterior repair – reinforces the back vaginal wall for rectal support
Uterine suspension – for uterine prolapse, preserving the uterus when appropriate
Vaginal hysterectomy – if uterine removal is required
Vaginal vault suspension – for prolapse after hysterectomy
Dr. Tourani uses native tissue repairs, avoiding the use of synthetic mesh, and tailors each surgery to the patient’s anatomy and life stage.
A Thoughtful, Woman-Centred Approach
Dr. Affie Tourani takes time to listen to your concerns, explain your options clearly, and guide you through treatment with warmth and professionalism. She is committed to helping women restore pelvic support while preserving function, dignity, and comfort.
Recovery and Results
Most surgeries are performed vaginally, without external cuts
Hospital stay is usually 1–2 nights
Light activities can resume in 1–2 weeks
Full pelvic healing takes around 6 weeks
Long-term outcomes are excellent when combined with ongoing pelvic floor care