SURGICAL THYROID CONDITIONS
Understanding the Thyroid Gland
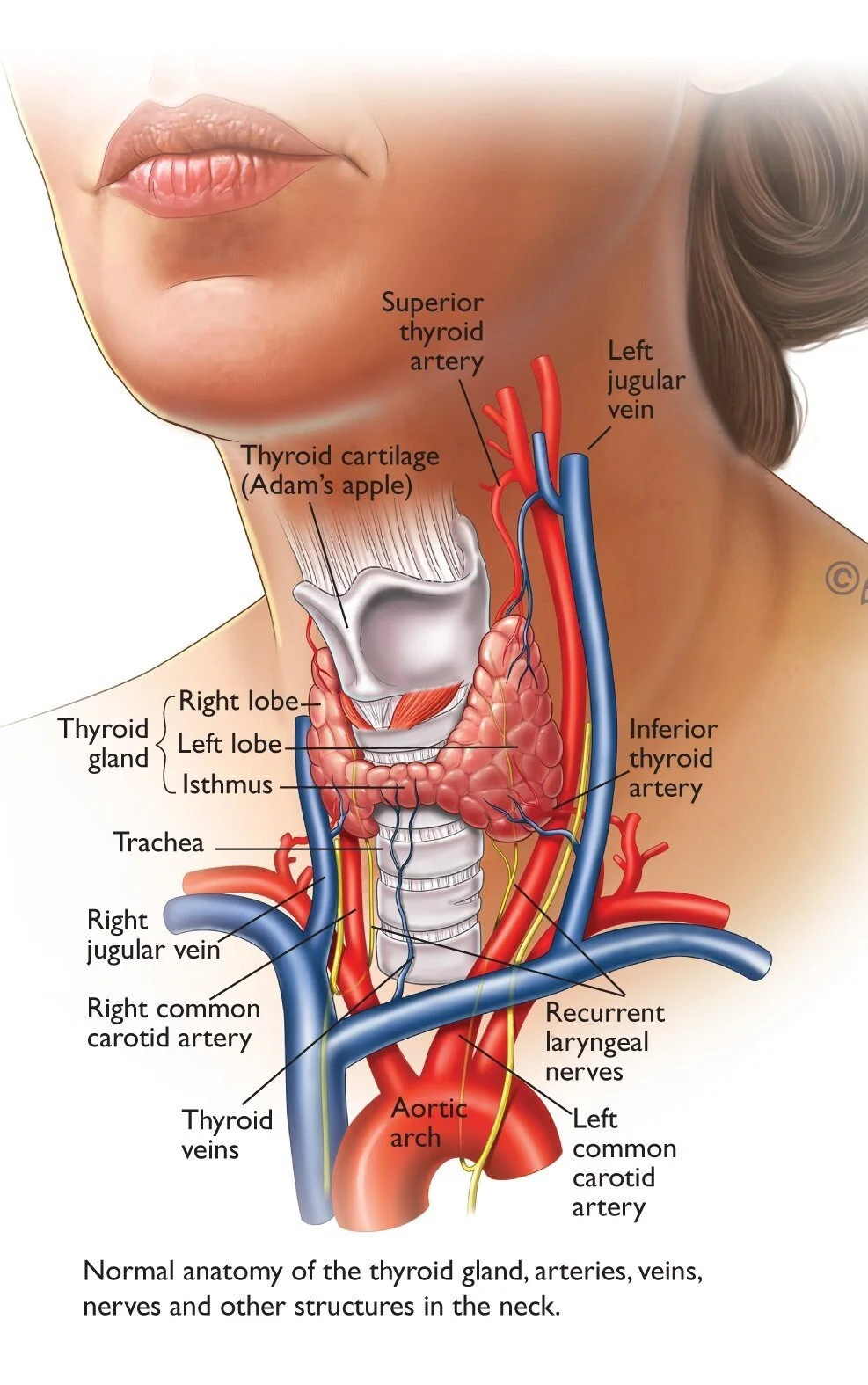
The thyroid is a butterfly-shaped gland located at the base of your neck. It plays a crucial role in regulating your body’s metabolism, energy levels, heart rate, and temperature through the production of thyroid hormones (T3 and T4). Thyroid conditions are common and can affect people of all ages. While many thyroid problems can be managed medically, some conditions require surgery, either due to the size of the thyroid, abnormal function, or concern for cancer.
Common Thyroid Conditions
Thyroid Nodules:
These are lumps or growths in the thyroid. Most are benign, but some can be cancerous or cause compressive symptoms like difficulty swallowing or a visible lump in the neck.
Multinodular Goitre:
When multiple nodules cause the thyroid to enlarge, it can result in cosmetic concerns, difficulty breathing or swallowing, or abnormal thyroid hormone levels.
Hyperthyroidism:
An overactive thyroid, commonly caused by Graves’ disease or toxic nodules, may require surgery if medications or radioactive iodine are not effective or suitable.
Thyroid Cancer:
Most thyroid cancers are highly treatable when detected early. Surgical removal is often the first and most important step in treatment, followed by tailored post-operative care.
When is Thyroid Surgery Recommended?
Surgery may be advised in the following situations:
Suspicion or confirmation of thyroid cancer
Large goitre causing compressive symptoms
Cosmetic concerns due to neck swelling
Persistent hyperthyroidism not controlled with medications
Indeterminate or suspicious biopsy results
Types of Thyroid Surgery
Surgical management is tailored to your specific condition, whether it’s benign nodular disease, hyperthyroidism, or thyroid cancer. The goal is always to achieve optimal disease control while preserving important surrounding structures, such as the nerves and parathyroid glands.
Hemithyroidectomy (Lobectomy)
This involves removing one lobe (half) of the thyroid gland. It is commonly performed when:
There is a solitary nodule with indeterminate biopsy results
The nodule is large or symptomatic but confined to one lobe
Low-risk thyroid cancer is confined to one side
Majority of the patients retain normal thyroid function with the remaining lobe and do not require long-term hormone replacement.
Total Thyroidectomy
Removal of the entire thyroid gland. This is indicated when:
Thyroid cancer is confirmed or strongly suspected
Multinodular goitre involves both lobes
Graves’ disease is not controlled with medical therapy
The patient prefers definitive treatment to avoid future procedures
Patients undergoing total thyroidectomy will need lifelong thyroid hormone replacement therapy.
Completion Thyroidectomy
This is performed when a hemithyroidectomy has already been done and a diagnosis of cancer is later confirmed on pathology. The remaining lobe is removed to reduce recurrence risk and facilitate radioactive iodine therapy and long-term monitoring using thyroglobulin.
Isthmusectomy
This is a more limited procedure involving removal of the isthmus — the thin bridge of thyroid tissue connecting the two lobes. It is only suitable when a small nodule is confined to the isthmus without any suspicious features elsewhere.
Note: “Nodulectomy” — the removal of just the nodule — is generally not recommended when the nodule is located outside the isthmus. Instead, a full lobectomy is performed. This ensures complete assessment of the surrounding thyroid tissue and avoids the need for reoperation on the same side, which carries a higher risk of injury to the voice nerve due to scarring from prior surgery.
Lymph Node Dissection for Thyroid Cancer
Papillary thyroid cancer (PTC) commonly spreads to lymph nodes in the neck, often at an early stage. As part of comprehensive surgical management, removal of involved lymph nodes may be necessary to reduce the risk of recurrence and support accurate staging.
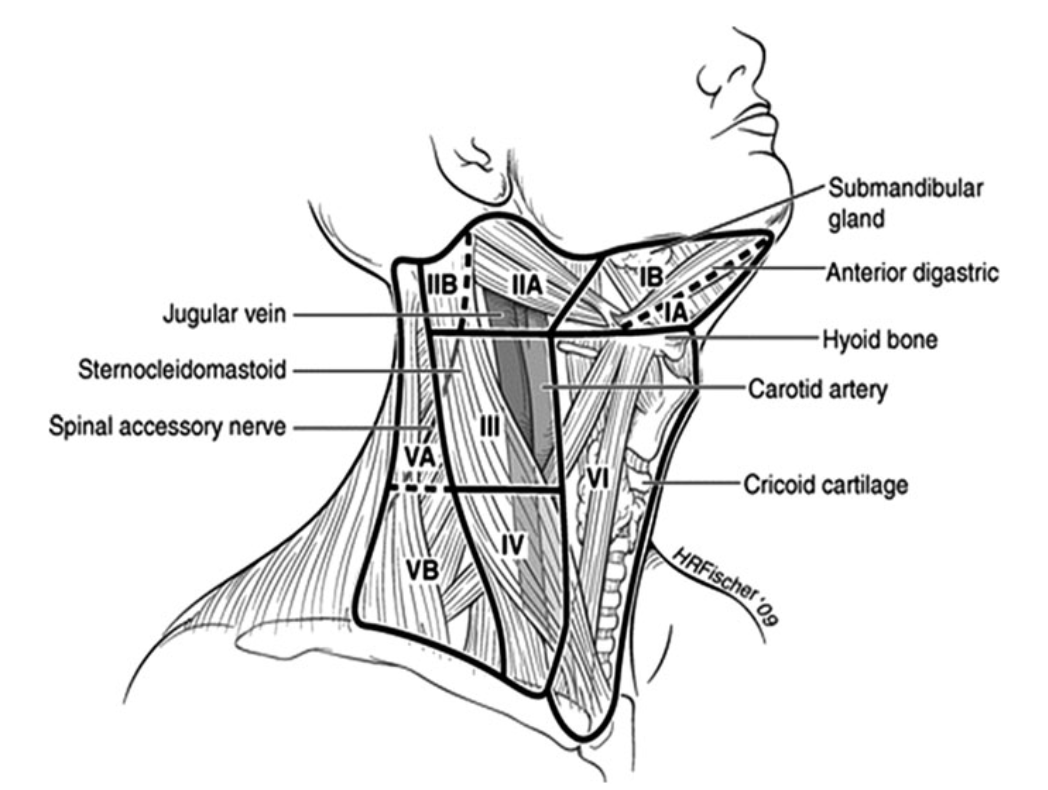
Central Neck Dissection (Level VI)
This involves removal of lymph nodes located directly behind and around the thyroid gland, in the central compartment of the neck. • In PTC, prophylactic central neck dissection is often recommended on the same side as the cancer, even if the nodes appear normal on imaging, due to the high risk of microscopic involvement.
Lateral Neck Dissection (Level II-V)
This refers to the removal of lymph nodes along the side of the neck. Lateral neck dissection is only performed when there is clear preoperative evidence of nodal involvement, typically confirmed by imaging and fine-needle aspiration biopsy. It is a more extensive procedure requiring meticulous technique to preserve nearby nerves (including the accessory and vagus nerves), major blood vessels, and other vital structures.
These procedures are only recommended when there is a clear benefit. I carefully assess each case with preoperative imaging and, when needed, fine-needle aspiration to ensure the surgical approach is both safe and appropriate.
Risks of Thyroid Surgery
Thyroid surgery is generally safe and well-tolerated, particularly when performed by an experienced endocrine surgeon. However, like all surgical procedures, there are potential risks. These are uncommon, and I take every measure to minimise them through precise technique and intraoperative monitoring.
1. Voice Changes or Hoarseness
The recurrent laryngeal nerves, which control the vocal cords, run close to the thyroid gland. Temporary voice changes can occur in up to 10% of patients due to nerve irritation, and permanent voice changes are rare (less than 1%).
I use a nerve monitoring device and magnification during surgery to protect this delicate structure.
2. Low Calcium Levels (Hypocalcaemia)
The parathyroid glands, which regulate calcium levels in the body, are located just behind the thyroid. Each thyroid lobe typically has two parathyroid glands. If their blood supply is disrupted during surgery, it can lead to low calcium levels (hypocalcaemia). This is a potential risk after a total thyroidectomy, as all four glands may be affected, but it is extremely unlikely after a hemithyroidectomy, since the parathyroid glands on the opposite, untouched side continue to function normally.
In most cases, this is temporary and managed with supplements.
Permanent hypocalcaemia is rare, affecting up to 5% of patients.
I take special care to preserve the parathyroid glands and their blood supply, and re-implant any that appear at risk.
3. Bleeding or Neck Haematoma
Bleeding is rare but can be serious if it causes pressure in the neck. I use meticulous techniques to ensure complete haemostasis.
Most patients go home safely within 24 hours.
In very rare cases, emergency intervention may be required.
4. Wound Infection or Poor Healing
Infections are uncommon due to the clean nature of neck surgery. You’ll receive appropriate post-op instructions to keep the wound clean and support healing.
5. Scar Formation
Thyroid surgery is performed through a low neck incision. In most people, the scar fades well over time. I place incisions in natural neck creases and use meticulous closure techniques to optimise the cosmetic result. Silicone gels or laser treatment can further improve scar appearance if needed.
6. Anaesthetic Risks
As with any surgery, there are general risks related to anaesthesia, especially in patients with underlying health conditions. These will be discussed with you before your procedure, and your anaesthetic care will be managed by experienced specialists.
Pre-Operative Evaluation
As part of my commitment to precise and personalised care:
I perform a high-resolution ultrasound myself during the consultation.
I use fine-needle aspiration biopsy (FNA) when needed to assess nodules.
Additional imaging (e.g., CT, MRI) or nuclear medicine scans may be arranged if required.
I collaborate closely with your GP and endocrinologist to ensure a coordinated approach.
For further details on assessment and management of thyroid nodules please check out my dedicated blog on this topic. .
Blog: Thyroid Nodules
Surgical Approach & Recovery
Most thyroid surgeries are performed under general anaesthesia and take 1–2 hours. My techniques aim to:
Minimise scarring (often a small incision in a skin crease)
Preserve the recurrent laryngeal nerves and the external branch of superior laryngeal nerve and your vocal function.
Identify and preserve the parathyroid glands (to avoid calcium imbalance)
Recovery:
Hospital stay is usually 1 night.
Most patients return to work or normal activities within 1–2 weeks.
You may need lifelong thyroid hormone replacement if the entire gland is removed.
Minimising Risk Through Expertise
Thyroid surgery requires more than just technical skill — it demands a comprehensive and thoughtful approach. I place a strong emphasis on thorough preoperative assessment, taking the time to understand the nuances of your condition through careful review of biochemical tests, advanced imaging, bedside ultrasound, and, when appropriate, fine-needle biopsies.
Every aspect of your care is tailored to your individual diagnosis and goals, with a high degree of attention to detail at every step. In the operating theatre, I use meticulous technique to preserve function and minimise complications.
Equally important is the compassionate, patient-centred care you receive before and after surgery. I ensure that you are well-informed, supported, and confident throughout your treatment journey. My goal is to deliver not just a successful operation — but a smooth, safe, and reassuring experience from beginning to end.
Other Useful Links
Thyroid Patient Information from American Thyroid Association: https://www.thyroid.org/thyroid-information/
Thyroidectomy: https://www.healthdirect.gov.au/thyroidectomy